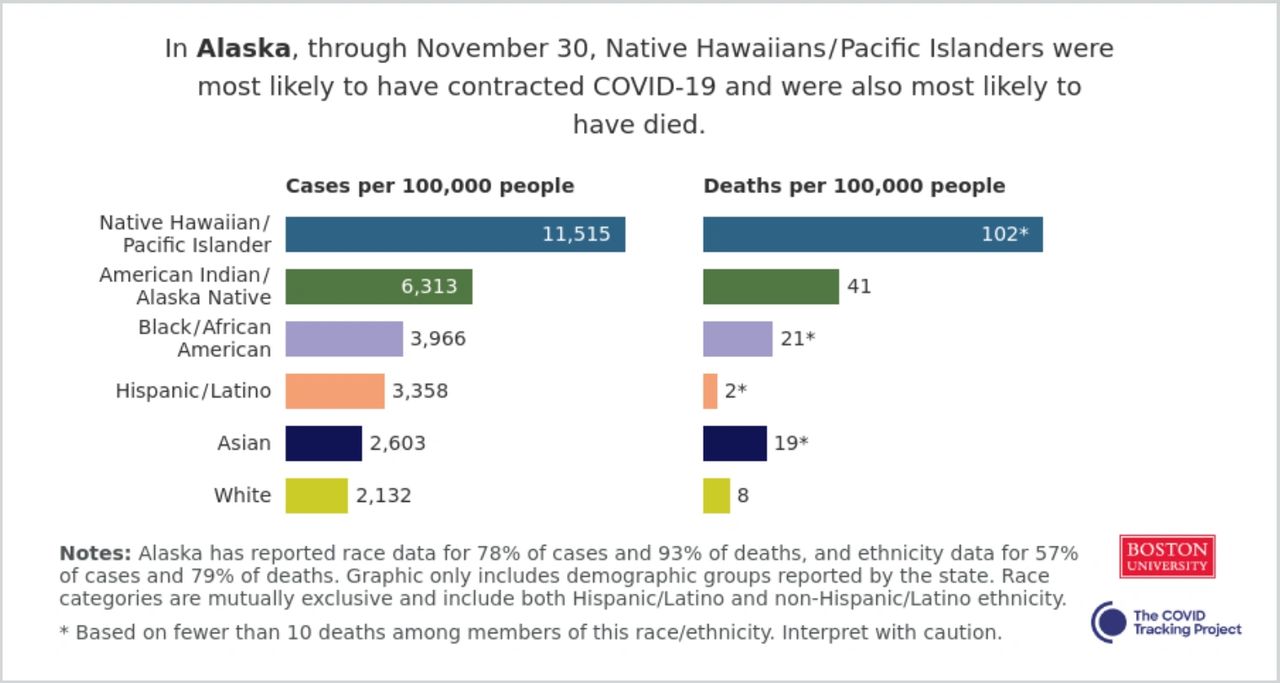
Alaska, COVID-19 and Race by Data
According to data supplied by the state of Alaska, through November 30, Native Hawaiians/Pacific Islanders were the most likely group of people to have contracted COVID-19 and were also most likely to have died. American Indian/Alaska Natives make up the second largest group of people directly affected by COVID-19 with 6,313 cases per 100,000 people. Black/African Americans were the third largest group affected by the pandemic followed by Hispanics/Latinos and Asians. White people rank last in the state, according to data.

Alaska Chief Medical Officer Dr. Anne Zink participated in an online Zoom conference with the Alaska Black Caucus last month discussing the topic of ethnic and racial disparity. Dr. Zink demonstrated effectively that minority groups in Alaska are indeed disproportionately affected by COVID-19 within the state.
According to the most recent data available, American Indian/Alaska Natives comprise 14% of Alaska's population and 27% of COVID-19 cases within the state. The same group accounts for 39% of the total number of COVID-19 deaths in the entire state of Alaska.
Native Hawaiians and Pacific Islanders Account for just one percent of Alaska's population and account for 8% of the states COVID-19 cases and 4% of deaths.
A study published in the Official Journal of the American Academy of Pediatrics Children's National Hospital in Washington, DC, analyzed COVID-19 data from 1,000 patients referred to a pediatric drive-through and walk-up testing site from Mar 21 to Apr 28. The study concluded that when children tested for SARS-CoV-2 through a community-based testing site, racial and/or ethnic minorities and socioeconomically disadvantaged children carried the highest burden of infection.
Rohan Khazanchi and Jasmine Marcelin, MD, of the University of Nebraska, and Charlesnika Evans, Ph.D., MPH, of Northwestern University, say that racism rather than race is behind COVID-19 racial health inequities." The elevated incidence of COVID-19 among Black and Hispanic communities, largely attributable to social and structural vulnerabilities, seems to drive the differences in mortality among Black, Hispanic, and White populations," they wrote also adding, "In short, rather than validating long-debunked hypotheses about intrinsic biological susceptibilities among non-white racial groups, the evidence to date reaffirms that structural racism is a critical driving force behind COVID-19 disparities."
What We Can Do
The Centers for Disease Control and Prevention says that community and faith-based organizations, employers, healthcare systems and providers, public health agencies, policy makers, and others all have a part in helping to promote fair access to health. To prevent the spread of COVID-19, we must all work together to ensure that people have resources to maintain and manage their physical and mental health, including easy access to information, affordable testing, and medical and mental health care. We need programs and practices that fit the communities where racial and minority groups live, learn, work, play, and worship.
You can read more about what we can collectively do to help minimize the disproportionate impact COVID-19 has on Alaska here.